More people are seeking care, but there aren't enough therapists: How can we work together to tackle this crisis?


In the past mental health was a taboo topic in mainstream media. Thankfully, these taboos have broken down in recent years. From celebrities opening up about their struggles to high-profile education and awareness campaigns, public discourse around mental health has become far more widespread and inclusive than it once was.
People are beginning to feel more empowered to speak up rather than suffer in silence. As a result, more people are seeking mental health support than ever before. However, the sad reality is that the U.S. healthcare systems lack the infrastructure and resources to support this growing demand.
As the need for care has risen, the supply of available therapists has actually diminished. The shortage worsened when the pandemic hit and hasn’t eased. Remote communities are taking a greater hit than their urban counterparts. “There are currently 111 million people living in therapist shortage areas. This is especially critical in rural communities,” said Seth Kutty, Head of Data Science for the Health Plan Group within Kaiser Permanente, during a recent webinar organized by Kintsugi: ‘Growing Spotlight on Mental Wellness: How technology must be a part of the solution for change.’
He was one of the four experts invited to participate in this discussion, which covered the therapist shortage and other key issues in mental health today. Other panelists included Dr. Michelle Drapkin, founder and director of the CBT Center and a board-certified clinical psychologist; Kristian Ranta, CEO and Founder of Meru Health; and Dr. Prentice Tom, Chief Medical Officer at Kintsugi.
The growing mental health crisis gripping our nation is showing no signs of slowing down, and the panel agreed that we must urgently address the therapist shortage now to prevent it from worsening. Three key themes emerged as solutions from the conversation.
Better stratification of mental wellness
When a patient is diagnosed with a physical health condition like cancer, their illness is stratified according to how advanced it is. This “staging” determines the treatment options available to the patient, and whether more aggressive measures such as surgery are necessary.
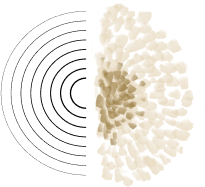
We lack “staging” when it comes to mental health. Our current system tends to treat people only when they’ve reached a crisis point (i.e., those with a clinical disorder). In this sense, mental health care is somewhat black and white: you either have a disease or you don’t. But mental health itself is far more complex than this: it is more of a spectrum than an on-off switch. There are multiple points along this spectrum where we can intervene and prevent people’s mental health from deteriorating long before it reaches a critical clinical state.
New technologies can facilitate this, including voice biomarkers – which are enabling a true paradigm shift in mental health. Just by listening to short clips of speech, this screening tool can determine how depressed or anxious a person is. In other words, it provides an overall mental wellness score. In addition, voice biomarkers are extremely accurate at detecting the presence of disease – “much more so than just talking to people,” Dr. Prentice Tom told us during the webinar. “Even when people are trying to hide it, or it's buried in their emotional state at that time, we can still pull out the psychiatric pathology from certain voice characteristics.”
The implications of this tech are huge: not only for healthcare systems, which can use it to gain a 360-degree view of a population's mental health, but also for individuals, who can better assess their own mental wellness and take action to promote it. In both cases, users are alerted about lapses in mental health no matter how “mild” they may seem. These early stages of mental distress are when we should be taking action. Just like physical health conditions, having tools that allow us to "stage" people's mental health can help determine what treatment options might benefit different patients—ultimately minimizing the need for more advanced treatments like a visit with a trained therapist.
When we implement this technology in a healthcare setting, “it will help us determine what treatments work for what people, so that we can eventually match people to treatments, which will bring a more personalized approach to mental health care,” said Dr. Michelle Drapkin.
Another promising long-term outcome will be a rise in people’s mental health literacy. A population that is more aware of its mental wellness is better equipped to address issues when they arise. This means more people will have the toolkit to self-treat, and fewer people will require specialized therapy.
Diverse solutions for diverse populations
Not everyone experiencing mental health issues needs a highly-trained therapist, yet at the same time, not everyone will benefit from just any treatment. There’s no blanket solution when it comes to mental health. We live in a diverse society with varied needs and need a range of therapeutic options to reflect this.
We’re seeing an explosion in the mental health tech space. Many chatbots and virtual therapists have become available in recent years, offering patients round-the-clock support and valuable coping strategies. But it’s essential to ensure that these new solutions cater to everyone. “Younger generations feel more comfortable using apps and tech, but we need many solutions available for all the different segments of society,” including older people and other marginalized populations, Seth Kutty pointed out during the online discussion.
Addressing the mental health of the entire population requires a “multi-pronged approach,” Dr. Prentice Tom added. “It's an enormous issue, but if we look at certain groups one by one, it's more achievable.” We can use different points of contact to reach diverse populations. To list a few: maternal mental health care during routine pre- and postnatal checkups, workplace initiatives to combat burnout – a leading driver of mental illness, or programs teaching school-aged kids about healthy social media use.
Journaling is one solution that's accessible for just about all of these populations. The act of unloading thoughts onto paper alone can be highly therapeutic. But the real “superpower” that journaling gives people is the ability to recognize triggers, detect patterns in their thinking, and notice when they are making positive progress. Voice journaling takes this a step further. People can speak as they would to a therapist or friend. Kintsugi’s mental wellness voice journaling app (link) gives people real-time feedback about their mental wellness score, so users can even better identify when they need to take action.
What does taking action look like? “It's all about learning skills and techniques so that you can self-regulate,” Kristian Ranta explained. “For example, certain breathing practices can regulate your nervous system, which gives you the power to control some of your responses during a panic attack.”
Incentivize careers in mental health
Even in the best-case scenario of more (and varied) therapeutic solutions and better mental health literacy across the population, there will still always be a need for mental health professionals. The current shortage is expected to worsen: by 2025, the US Department of Health and Human Services predicts that there will be 10,000 fewer mental health professionals than needed.
We need to take measures now to recruit more mental health professionals. This will start with recruitment drives “just like we’ve done with electrical engineering and nursing – when the correct incentives are put in place, a lot more people join these professions,” Dr. Prentice Tom observed.
These initiatives to attract people to mental health careers must be backed by better incentives. For example, Kristian Ranta pointed out: “We have state networks of therapists, and it’s currently very difficult to change licenses to different states. This is just one example of red tape that can make therapists’ jobs more difficult. Of course, it's there for a reason, but we have to recognise that the world is changing, and requirements and needs are different now.”
Most of these solutions are available right now. We need to work together to raise awareness and promote a better collective understanding of the universe of mental health tools – from technological solutions like apps to natural coping strategies like breathing exercises. None of these things can or will replace mental health professionals, but they can go a long way in helping people better manage and measure their mental wellness.
Tune into the full recording here:
Join our mailing list for regular updates from Kintsugi